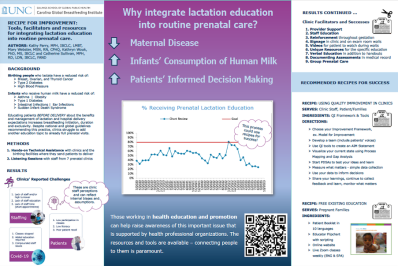
Recipe for improvement: Tools, facilitators and resources for integrating lactation education into routine prenatal care.
Authors: Kathy Parry, MPH, IBCLC, LMBT1, Mary Webster, MSN, RN, CPHQ2, Kathryn Wouk, PhD, MS, IBCLC3 and Catherine Sullivan, MPH, RD, LDN, IBCLC, FAND1
(1)Carolina Global Breastfeeding Institute at UNC Chapel Hill, Chapel Hill, NC, (2)Population Health Improvement Partners, Calabash, NC, (3)PIRE Chapel Hill, Carrboro, NC
Quality Improvement Tools
Special Sauce Tips to Starting Improvement Projects in a Clinic Setting
- Don’t re-create the wheel: Start talking with professional orgs, other clinics (same size, regions, larger, national) to see what’s working well & what’s easily replicable. You are looking for “better ideas”, not just evidence-based practices.
- Providing Continuing Education “Carrots”: Although not imperative, health professionals appreciate & often need opportunities for practice-based CE/CME. Reach out to professional organizations for information on improvement grants, local foundations, area AHECs, and CME/National Boards for QI/CME funding support.
- Check your project scope: Start researching if financial support is necessary due to scope of project (i.e., wanting an improved process for all patient education, not just a sole focus on prenatal).
- Cause for Improvement: When you’re ready to “pitch” improvement work, as simply as possible, collect feedback on the process to improve, attach with current EBP. Focus on the System problems not People problems. Offer solutions early and frequently.
- Gathering a Team of partners: Find a like-minded audience to garner the WILL & excitement to do the work. Your audience will become a partner in recognizing areas for improvement, prioritizing solutions, testing and implementing solution
- What we don’t see: Talk with staff who’ve been recent “expectant moms” who can speak to processes; informal discussions with current patients via focus groups, surveys, etc. *Don’t forget to add a patient/client to your team- one who receives the service(s).
- Framework for Success: Consider using a proven yet simple framework for your improvement work- Model for Improvement, PDSA cycles, and simple data collection tools. Learn more by viewing the accompanying QI Toolbox videos.
Just in Time Videos (via Improvement Partner’s YouTube Channel; each approximately 4-10 mins in length)
- Model for Improvement
- PDSA
- Process Mapping
- Fishbone Diagram
Lactation Education Resources for Prenatal Offices
Ready Set Baby (Patient Booklet and Scripted Educator Flipchart)
- Available in Spanish, French, Arabic, Chinese, Burmese, Nepalese, Uzbek, Russian and Ukrainian
- Free printable PDFs – choose your preferred printer
- Evidence-based, pilot tested
Ready Set Baby Online (website version of patient booklet)
- Available in Spanish and Arabic translations
Ready Set Baby Live (free weekly live Zoom classes)
- Available in English and Spanish
Poster References
- Crowe, S. D., & Hanley, L. E. (2018). Optimizing support for breastfeeding as part of obstetric practice. Obstetrics and Gynecology, 132(4), E187-E196.
- Kilpatrick, S. J. (Ed.). (2017). Guidelines for perinatal care. American Academy of Pediatrics.
- World Health Organization. (2020). Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services: the revised Baby-friendly Hospital initiative: 2018 implementation guidance.
- Wouk, K., Tully, K. P., & Labbok, M. H. (2017). Systematic review of evidence for baby-friendly hospital initiative step 3: prenatal breastfeeding education. Journal of Human Lactation, 33(1), 50-82.
- WHO & UNICEF Global Breastfeeding Collective. (2022). Global Breastfeeding Scorecard. Percent of Caregivers Counselled in IYCF Indicator and Inclusion of IYCF Support in Pre-Service Curricula Indicator. https://www.globalbreastfeedingcollective.org/global-breastfeeding-scorecard
- Breastfeeding Benefits Both Baby and Mom. (2023) https://www.cdc.gov/nccdphp/dnpao/features/breastfeeding-benefits/index.html