Mapping the journey to adopt glucose monitoring technology among older adults with Type 1 diabetes
February 3, 2023
New research from the UNC Gillings School of Global Public Health could give health care providers and scientists the insights to assist older adults in adopting new technology to manage Type 1 diabetes.
Published in Diabetes Research and Clinical Practice, the new study maps the unique and complex journey that patients 65 and older face when using continuous glucose monitoring (CGM) and helps clinicians and other members of the care team, such as diabetes care and education specialists, anticipate potential roadblocks to both taking up and continuing to use the treatment to achieve the best possible health.
The number of people over the age of 65 years living with Type 1 diabetes has increased over the past few decades. To manage their condition, they must closely monitor their blood sugar levels to avoid emergencies, specifically when blood sugar levels drop too low. CGM is an emerging treatment option for people with diabetes to monitor blood sugar levels throughout the day without the hassle of multiple finger sticks. By inserting a small glucose sensor under the skin, real-time glucose levels can be wirelessly transmitted to a monitor, which may connect to a receiver, an insulin pump, or a smartphone — all of which can alert patients when blood sugar levels are out of range.
While the technology has been shown to be helpful for diabetes management in all age ranges and especially effective at reducing dangerous episodes of low blood sugar in older adults, some older patients may have a hard time adjusting to technology as part of their diabetes management. While some barriers to adoption are well-known, previous research did not often describe the first-hand experiences of these patients.
The new study is the first of its kind to “map” the journey of CGM use among older adults and identify the multiple pain points that make it harder for them to stick with the treatment. Researchers used tools from the field of systems science to collaborate with older adults living with diabetes and their caregivers (those who assist them at home) to document each step of their experience with CGM, including the unexpected ways in which challenges and benefits may unfold.

Dr. Kristen Hassmiller Lich
“There’s a tendency to try and find simple solutions to complex health problems, but with older adults, we’re finding that it’s not so easy. It’s a set of challenges for each person,” said senior author Kristen Hassmiller Lich, PhD, associate professor of health policy and management at the Gillings School. “This new research shows that the decisions and processes surrounding technology use are not simple– there are different needs that providers have to consider when helping older adults with diabetes get started with CGM and sustain use of it.”

Dr. Anna Kahkoska
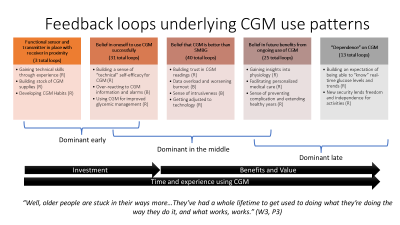
Those challenges could include the time and energy required to learn about new technologies, difficulty with inserting the sensor, navigating an onslaught of new glucose information, adjusting to alerts and alarms, and building trust in CGM readings. In total, the research team, led by Assistant Professor of Nutrition Anna Kahkoska, MD, PhD, identified more than 140 unique stories whereby an individual older adult’s experiences with CGM may reinforce or counteract their future use, called feedback loops.
Each story helps to shed light on potential challenges and benefits that come from adopting and using CGM, from the point of view of both older adult patients and caregivers. The researchers are focused, in particular, on the feedback loops that increase difficulty in adapting to the technology, as these may represent opportunities to help. Understanding the full picture of these loops can aid in designing and delivering personalized support as patients wrestle with different challenges over time.
The study team identified these feedback loops through a series of workshops that brought together older adults with T1D and caregivers to talk about their perceptions and experiences with CGM. The workshops allowed the participants to collaboratively identify the most critical issues that could hinder CGM use and brainstorm ideas to address them. The data taken from these workshops aided the research team in building a series of visual diagrams, or system models, that attempt to map the full spectrum of patient experiences.
According to Kahkoska and Hassmiller Lich, there have been very few studies that have used this participatory systems science method, called “group model building,” to collaborate with older adult patients in research that is relevant to their own health. This method can help researchers and caregivers understand the complexity of experiences that patients might have when managing their own care for a chronic disease like Type 1 diabetes in a holistic way.
“Our goal is to use this information as a framework for developing new interventions to better support older adults to incorporate technology as a part of their diabetes management,” Kahkoska said. “The system map is particularly helpful in detangling these complex experiences that people may have into feedback loops that we can more easily understand. It reveals opportunities to better match available resources to individual older adults as they navigate the learning curve of CGM, and ideally, pre-empt the challenges they may encounter.”
The full diagram of the model is available online as an interactive system map.
Kahkoska, who is a KL2 scholar at the North Carolina Translational and Clinical Sciences (NC TraCS) Institute, is currently leading a series of follow-up studies that will continue to engage older adults living with diabetes. The team will also collect data from health care providers, behavioral health scientists, community health workers and insurance providers to identify the highest leverage opportunities to help, including clinical and non-clinical ways of offering support. The long-term goal of this research is to ensure that all individuals living with diabetes have access to the time, training and support that they need to benefit from the technologies that are designed to help, regardless of their age.
Kahkoska is supported by the National Center for Advancing Translational Sciences at the National Institutes of Health (NIH) through Grant KL2TR002490. The project was supported by UL1TR002489 from the Clinical and Translational Science Award program of the Division of Research Resources at NIH and a research grant from the Diabetes Research Connection.
Contact the UNC Gillings School of Global Public Health communications team at sphcomm@unc.edu.