Study finds excess medical costs associated with metastatic breast cancer, especially among younger women
May 20, 2020
A study from the University of North Carolina at Chapel Hill has found that metastatic breast cancer is associated with substantial excess health care costs for patients.
Using statistical modeling based on insurance claims data, researchers estimated medical costs for patients with metastatic breast cancer. For comparison, they also estimated costs for patients with earlier-stage breast cancer and with no cancer who were in the same age group, from the same county of residence and who had the same type of health insurance.

Dr. Justin Trogdon

Dr. Stephanie Wheeler
The study’s co-authors include Justin Trogdon, PhD, and Stephanie Wheeler, PhD, both professors of health policy and management at the UNC Gillings School of Global Public Health and researchers at the Center for Health Promotion and Disease Prevention (HPDP) at UNC-Chapel Hill. It found that, across all age groups, average monthly costs were much higher for metastatic breast cancer patients than for earlier-stage cancer patients or those without cancer. The largest cost differences between metastatic breast cancer patients and other patients existed in the younger and midlife groups: ages 18 to 44 and ages 45 to 64, respectively.
“Our results highlight the tremendous cost burden associated with metastatic breast cancer among working-age women, particularly during the years after initial treatment of metastatic disease as well as at the end of life,” said Wheeler.
For women with metastatic breast cancer – where the five-year survival rate is only 26.3% compared to 98.8% for localized cancer – treatment continues for longer, and it includes end-of-life care. These factors contribute to the high medical costs associated with metastatic breast cancer, which can be a financial burden for women and their families.
The finding that medical costs are higher for younger and middle-age women may reflect their desire for more aggressive treatment and willingness-to-pay for additional months of life, the researchers point out, or it may reflect breakdowns in shared decision-making between patients and practitioners, leading to treatments with minimal financial or health benefits for patients.
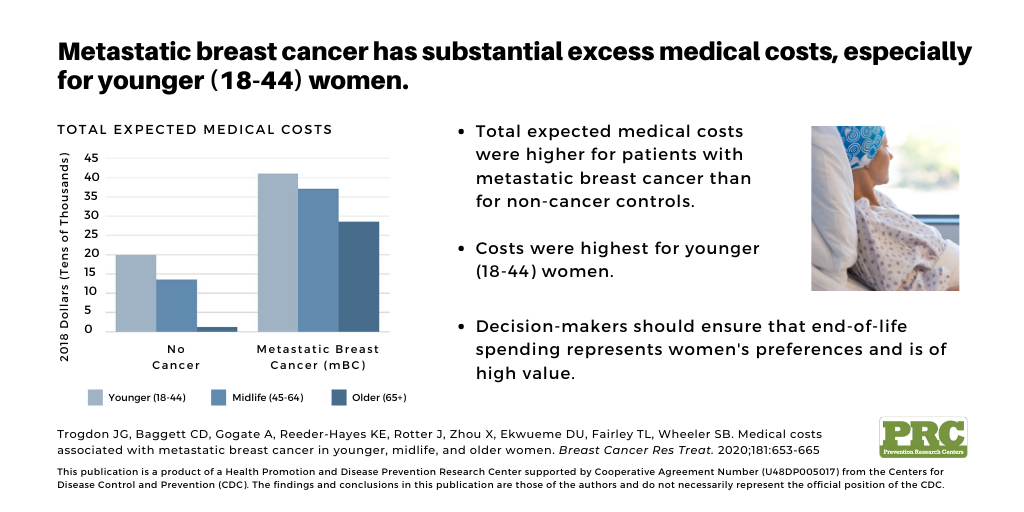
This chart illustrates the total expected medical costs per patient.
“Our results suggest that we spend nearly twice as much in the last year of life for women that die of breast cancer compared to other causes of death,” said Trogdon. “We should work to ensure that end-of-life spending for metastatic breast cancer represents women’s preferences and is of high value.”
By identifying the age groups and phases of care where medical costs are the highest, the results of this study may inform decision-makers about where to invest resources, for example, which groups of patients may be in need of extra financial or psychological support. The study can also inform future research into how to improve metastatic breast cancer treatment for populations or treatment phases that are currently associated with the highest medical costs.
Read the full article in Breast Cancer Research and Treatment.
Additional authors: Christopher D. Baggett, Anagha Gogate, Katherine E. Reeder-Hayes, Jason Rotter, Xi Zhou, Donatus U. Ekwueme and Temeika L. Fairley.
Contact the UNC Gillings School of Global Public Health communications team at sphcomm@unc.edu.
