Positive social ‘nudges’ could encourage more providers to treat opioid use disorder
November 3, 2021
Medication for opioid use disorder (MOUD) is an evidence-based treatment that can greatly reduce deaths from opioid overdose, but the number of providers qualified to administer this treatment is critically low, especially in rural areas where primary care providers may be the main source of behavioral health treatment.
Training more health care practitioners to administer MOUD could help more patients gain access to treatment, and positive social messaging may be an effective way to encourage providers to seek MOUD training, according to a new study from researchers at the UNC Gillings School of Global Public Health.

Dr. Marisa Domino

Dr. Sean Sylvia

Dr. Sherri Green
Published in Health Services Research, the study was led by Professor Marisa Domino, PhD, and Assistant Professor Sean Sylvia, PhD, from the Department of Health Policy and Management, along with Associate Professor Sherri Green, PhD, MSW, LCSW, from the Department of Maternal and Child Health.
“Receiving a waiver to prescribe buprenorphine, one of the medications to treat opioid use disorder, is one of the many demands on our primary care workforce,” said Domino. “We set out to determine if we could structure a set of incentives and messaging approaches that would increase our chances of encouraging busy primary care providers to participate in this learning collaborative.”
To learn more about what kinds of messages, or “nudges,” incentivized health care providers to enroll in MOUD training, the study team tested messaging strategies by sending letters to 15,835 primary care providers statewide in North Carolina inviting them to participate in an online learning collaborative. In particular, they wanted to learn whether providers were incentivized by the prospect of financial reimbursement for time spent at the learning collaborative or by pro-social messaging – a type of communication that encourages behavior that will benefit society as a whole at some cost to an individual.
Four versions of the recruitment letters contained nudges in the form of either pro-social messaging, financial incentives, both or neither.
The team found that these nudges dramatically increased the response rate from providers. Most effective was the combination of pro-social messaging – which used customized regional statistics describing the magnitude of the opioid overdose epidemic in each county – and the mention of funding to support providers’ time in training. Used together, this messaging strategy increased provider response by nearly 50 percent over the group that received no nudges. By contrast, pro-social messaging alone increased response by 27 percent, and financial incentives alone resulted in a six percent increase.
“The fact that financial and pro-social messaging reinforced one another suggests that merely highlighting the social need may be an inexpensive way to increase the return on investment in public subsidies encouraging providers to treat opioid use disorder,” Sylvia said.
Among the physicians, nurse practitioners and physician’s assistants in practices that replied to letter, physicians and nurse practitioners showed the highest response to the combination of pro-social and financial incentive messaging. Nurse practitioners, in particular, responded to the combination at a 61 percent higher rate than physicians.
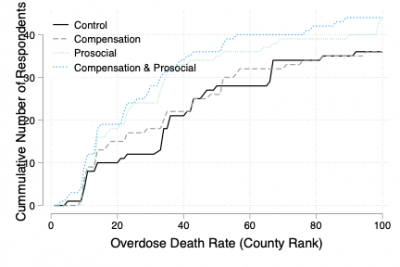
Response rate by county rankings by 2017 opioid overdose death rates
The customized regional statistics in the pro-social messaging led to a marked increase in response from counties that had higher rates of opioid overdose deaths.
“In N.C., with about 16,000 primary care providers, the estimated effect of pro-social messaging would translate to about 66 additional providers responding to the invitation,” the study team wrote. “Under fairly optimistic assumptions, if even half of this group receives a waiver and treats the initial 30 allotted patients, this would result in 989 additional people receiving opioid use disorder treatment for the modest cost of adding pro-social information to the invitation.”
The study team is planning future work to test other methods of nudging provider and patient behavior with the goal of increasing the treatment options for people with behavioral health conditions.
Contact the UNC Gillings School of Global Public Health communications team at sphcomm@unc.edu.
