Hospital closures in rural communities lead to longer ambulance drives
February 4, 2020
Emergency medical services (EMS) can often be the difference between life and death in critical health care outcomes, especially in acute cases like heart attack or stroke. People in rural areas of the United States wait, on average, nearly twice as long for ambulances as those in urban areas. New research from the UNC Gillings School of Global Public Health has found that hospital closures in rural areas increase those EMS transport times.
Many rural hospitals struggle to remain financially viable, and hospital closures are becoming more and more common in these areas. This puts a population that already experiences longer wait times for acute medical care even more at risk for poor health outcomes, not only because the distance between the patient and the nearest hospital increases, but also because hospital closures often mean the hospital-based EMS agency may also close. This requires the 9-1-1 dispatcher to notify an EMS agency that may be farther away from the patient.
Katherine Miller, MSPH, doctoral student and graduate teaching assistant in health policy and management at the Gillings School, is first author on a study that sought to quantify the effect of these closures on EMS response and transport times. The study, published recently in Health Services Research, also includes work from doctoral student Hailey James, MHA, and Professor Mark Holmes, PhD, both of health policy and management.
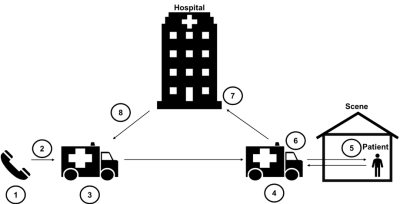
Timeline of a 9-1-1 call: 1) Time 9-1-1 call is made. (2) Dispatch notifies EMS unit of 9-1-1 call. (3) EMS unit is en route to the patient incidence where the 9-1-1 call was made: the scene. (4) EMS unit arrives at the scene. (5) EMS unit arrives at patient side. (6) EMS unit departs scene. (7) EMS unit arrives at destination. (8) EMS unit returns to service, i.e. ready to accept next call.
Because timely and appropriate response is important, EMS records include thorough data about EMS behavior through the lifecycle of a 9-1-1 call, beginning from the time a call for help arrives at 9-1-1 dispatch until the EMS team returns to service after the completion of an encounter with the patient. This data is tracked through the National Emergency Medical Services Information System (NEMSIS).
Through a retrospective cohort study that examined EMS transport times, response times and total activation times (the total amount of time elapsed from a 9-1-1 call to a completed encounter), Miller’s team compared pre- and post-hospital closure EMS times in areas designated by NEMSIS as rural or wilderness ZIP codes. They compared these times to patient encounters in rural or wilderness ZIP codes that did not experience a hospital closure after controlling for baseline differences between those that had a closure and those that did not.
The study found that in the year a hospital closed in a rural area, the average EMS transport and activation times increase. The closure did not affect average EMS response times. EMS transport times increased by an average of 2.6 minutes, and EMS activation times increased by an average of 7.2 minutes. In the subsequent year post-closure, the study found that transportation times increased by 4.7 minutes, and total activation time increased by 9.5 minutes as compared to the year prior to closure.
While these increases may seem small at first, evidence in previous studies has shown that even one-minute increases in EMS times could raise the chances of patient mortality.
According to the study’s descriptive analysis, “the average times in rural areas are already greater than 8 minutes. Best practices suggest that system response time should be equal to or less than 8-9 minutes. Given that minutes are critical in emergency medicine, these findings, in addition to the increase in times due to a closure, suggest rural hospital closures may further delay medical care to patients already experiencing mean wait times outside the gold standard.”
While the results of this study emphasize the need for timely EMS response in rural areas, they are also important because this data could help policymakers design solutions that better support hospitals in rural areas. Ensuring that patients have access to these critical services may factor into policy decisions regarding financial investments, both for rural hospitals and their local EMS agencies.
“This study provides evidence of the impact of rural hospital closures on the timely provision of emergency medical services,” said Miller. “Given the increasing number of rural hospital closures, investments in and optimal reimbursement policies for local EMS agencies should be considered to ensure rural communities maintain access to EMS in the event of an emergency.”
Contact the Gillings School of Global Public Health communications team at sphcomm@unc.edu.
