Clinical Scholars leadership training creates new opportunities to advance health equity
September 8, 2022
New findings from UNC-Chapel Hill are shedding light on the ways that inclusive leadership training can support institutional change and reduce the racial inequities perpetuated by health care systems.
Since 2016, researchers at the UNC Gillings School of Global Public Health and the UNC School of Medicine have directed the Clinical Scholars program, which gives health care providers the tools necessary to create actionable policies and practices that promote health equity.
These strategies have been gaining more and more attention since the spring of 2020. While many professional and educational organizations have made statements of renewed commitment to social justice in health care, these efforts are often led by small groups of people seeking to drive broad institutional change.
The Clinical Scholars program, with support from the Robert Wood Johnson Foundation, aims to help these change-makers create a lasting impact through three years of mentoring, networking and leadership curriculum. They have supported more than 150 fellows and 44 projects across 28 states and territories.

Dr. Giselle Corbie

Dr. Claudia Fernandez
Program co-directors Giselle Corbie, MD, MSc, and Claudia Plaisted Fernandez, DrPH, MS, RD, LDN, led the development of a case study, published recently in the Journal of General Internal Medicine, that describes how the first cohort of Clinical Scholars was able to grow their skills to advance health equity. The program’s framework, which focuses on 25 core competencies of leadership, includes eight competencies related to equity, diversity and inclusion (EDI).
Over the course of three years, 27 participants in the program – who came from sectors that included medicine, nursing, social work, dentistry and pharmacy – were measured on their self-reported level of knowledge, attitude, self-efficacy and intention to use the eight EDI competencies:
- Practice of multiculturalism
- Organizational capacity for advancing health equity
- Diversity and inclusion
- Health equity
- Meaningful community engagement
- Social determinants of health
- Commitment to inter-cultural development
- Social justice
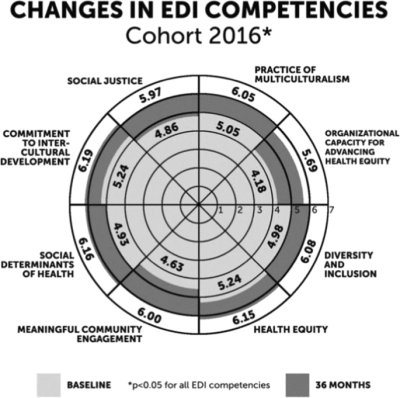
Self-Reported changes in EDI competencies of Clinical Scholars cohort 2016 participants
Results showed that participants demonstrated significant growth in all eight competencies. While most in the program already had some training or interest in EDI concepts, the program allowed many of them to evolve their understanding of personal bias or gain awareness of previously unexplored topics.
Participants also tracked and reported examples of how they implemented the competencies in their work while in the program. This included advocating for institutional policies and organizational structures, fostering inclusive environments, creating easier access to resources, engaging with the community, and training others.
After graduation, participants continued to report activities that fostered EDI: giving interviews on podcasts or at events, expanding programs to increase access to necessary care services, leading training initiatives, and authoring research. Some were recognized with honors for their outstanding commitment to EDI or grew their careers through advocacy work.
“Health disparities have been exhaustively examined as a deficit of individual inaction with a nod to structural inequities. We need more solutions-based public health efforts that leverage action,” the research team stated. “Equity-centered leadership training is one of the tools needed to address racial inequities. This case study describes how intense interdisciplinary leadership development prepares health care system leaders to work together and within systems to adapt and create organizational practices and policies that are congruent with health equity.”
According to the researchers, the findings in this case study are based on leadership development under the “normal stressors” that occurred prior to COVID-19. The team has published on pivots to support cohort connectedness and leadership development during the volatile, uncertain, complex and ambiguous times of the pandemic. Additional leadership topics may examine team leadership, the skills leaders lean into during the most uncertain of times and adaptation of the model with new team configurations.
The equity-centered model is now being piloted with community-academic teams working in rural North Carolina through Whole Community Connection.
Read the full case study online.
Study authors include Corbie, Gaurav Dave, MD, DrPH, and Melissa Green, DHSc, MPH, from the School of Medicine; Kathleen Brandert, MPH, from the University of Nebraska Medical Center; Cheryl Noble, MSPH, MSW, a leadership evaluation consultant; and Ellison Henry, MPH, Rachel Berthiaume, MPH, and Fernandez from the Gillings School.
Contact the UNC Gillings School of Global Public Health communications team at sphcomm@unc.edu.
