Collaborative lab environment leads to major weapon in Zika fight
December 1, 2016
It was nearly impossible to look at any news source in the first eight months of 2016 without coming across one single word, over and over again. Zika.
Mosquito-borne, rapidly spreading, with horrible potential impact upon pregnant women and their unborn children, Zika had no preventive vaccine, no treatment, no cure.
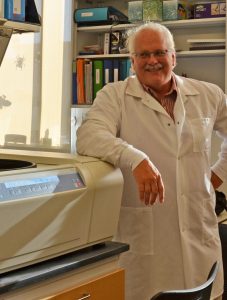
Dr. Ralph Baric (above) and his team showed how antibodies from Dengue fever survivors can be used to fight Zika. (Photo by Linda Kastleman)
Hope arrived earlier this year, thanks to a team led by Ralph Baric, PhD, professor of epidemiology at the University of North Carolina’s Gillings School of Global Public Health. The Baric team conducted research that showed how antibodies from patients who survived Dengue fever can be used to fight the Zika virus now. That could open the door to develop a Zika therapeutic treatment in the not-too-distant future.
The research was published July 19 in mBio, the journal of the American Society for Microbiology.
This rapid breakthrough came together as a direct result of the way Baric manages his lab, including the cultivation of innovation and inquiry by students and staff members in his group.
“Dr. Baric encourages us to stretch ourselves mentally and get outside our intellectual comfort zones,” says Jessica Plante, PhD, a postdoctoral fellow in the Baric lab and co-first author of the study.
Zika virus has been known since 1947 but was rarely studied, as human disease cases and outbreaks were rare. Then, something changed. First seen in an outbreak in Micronesia in 2007, Zika made its presence known throughout the world after surfacing in Brazil in late 2015, causing widespread concern, especially for the 2016 Olympics.
Outbreaks have been reported since in 46 countries. The virus is associated with severe neurological birth defects and fetal loss in pregnant women and the onset of Guillain-Barre syndrome in some adults.
As news spread about the virus, Plante and her fellow researchers became intrigued. Zika is a flavivirus, similar to viruses that cause Dengue fever, West Nile fever and yellow fever, all of which have been studied extensively by the Baric lab and its collaborators.
“Several of us knew that our lab and the virology research community at UNC were in a uniquely strong position to address it,” she says.
Plante discussed the outbreak with her colleague, Jesica Swanstrom, BS, who then approached Baric with an idea.

Dr. Ralph Baric (left) chats with research team members Dr. Jessica Plante (center) and Jesica Swanstrom. (Photo by Linda Kastleman)
“I asked him whether I could do a preliminary experiment based on a hypothesis constructed from the literature,” says Swanstrom, who works as a research specialist in the Baric lab. “That first assay yielded some interesting results, so Jessica Plante and I sat down together and designed some follow-up experiments that we wanted to perform.”
The work they would be undertaking was highly complex. In people who have contracted Dengue virus, antibodies generated by the body in response to serial infections may be protective or, under some circumstances, actually may promote more severe disease symptoms.
“We wanted to know how these pre-existing Dengue antibodies in the human population were likely to interact with the Zika virus,” Swanstrom says. “Would it protect people from infection, do nothing or exacerbate the condition?”
Conducting such a large-scale analysis at the cellular level presented a unique challenge. Then again, the Baric lab had a unique advantage – they had developed a proprietary reverse genetics system for Dengue virus that permitted such novel investigations.
Plante and Swanstrom designed experiments testing various monoclonal Dengue antibodies. After several sample runs, one antibody kept appearing as effective – EDE 1. Not only could it protect multiple cell types from infection in the lab, it also could do so in mice.
“We double- and triple-checked everything very carefully,” Baric says. “Each time, the same outcome occurred. The antibody derived from Dengue survivors, EDE 1, neutralized the Zika virus in cell cultures, creating a protective effect. A therapeutic treatment using these antibodies would protect pregnant women and others from contracting the Zika virus if they came in contact with it.”

It was well into 2016 before the team confirmed their findings – just as the media and public health warnings were becoming more pervasive. Olympics events were only a few months away, and mosquitoes carrying the disease had been found throughout South and Central America, the Caribbean and parts of the southern United States.
The finding is potentially a major advance for the prevention and treatment of Zika. Therapeutic antibodies generated from people infected with Dengue would be less likely to cause complications in patients infected with either virus. The treatment would not create a lifelong immunity but would be an effective short-term tool to prevent infections from the current strains of the Zika virus during an outbreak.
“[The potential value of our work] added a sense of urgency to what we were doing and caused us to be specific when writing the paper,” Plante says. “There were a lot of late nights and weekends, but I am proud that, at every step, we were appropriately cautious and precise.”
The resulting paper, “Dengue Virus Envelope Dimer Epitope Monoclonal Antibodies Isolated from Dengue Patients Are Protective against Zika Virus,” was published in the July/August issue of mBio, with Plante and Swanstrom as co-first authors.
The paper generated extensive media coverage and much discussion in the research community. Still, Baric took care that the results were not misinterpreted.
“Our findings did not mean that all Dengue survivors have protection against Zika,” Baric says. “In fact, we found only a small percentage of those people will have developed antibodies that have potential to protect against both viruses. However, this particular class of human monoclonal antibodies from a few DENV-infected individuals are potentially therapeutic and can prevent Zika virus infection.”
.

Dr. Ralph Baric

Dr. Jessica Plante

Jesica Swanstrom
Baric adds that additional testing will be required to further refine any treatment, such that it can combat the inevitable mutations of the Zika virus that will develop as more outbreaks occur.
“Follow-up studies with EDE1 and Zika in mouse models are a priority,” Plante says. “It still needs to be determined exactly how much EDE1 antibody is necessary for protection and whether the antibody still protects if it is administered after infection.”
Plante adds that other topics to explore include whether EDE1 is safe to administer during pregnancy and whether EDE1 can prevent Zika-associated birth defects.
Swanstrom adds that the discoveries would not have been possible if not for Baric’s leadership and the culture he curated in his lab.
“Dr. Baric is incredibly receptive to ideas for experiments and projects,” she says. “He has created an environment in which each team member is encouraged to try to incorporate genetics, immunology, virology and bioinformatics into our projects to develop more complete explanations for our observations.”
Thanks to Baric, Swanstrom says, the team is working on a variety of projects, all of which make for interesting science.
—David Pesci
Carolina Public Health is a publication of the University of North Carolina at Chapel Hill Gillings School of Global Public Health. To view previous issues, please visit sph.unc.edu/cph.
