How can we improve health and health care in rural America?
October 15, 2017
Mark Holmes, PhD
Associate professor of health policy and management
Director, UNC Cecil G. Sheps Center for Health Services Research
George Pink, PhD
Humana Distinguished Professor of health policy and management
About 46 million people – 15 percent of the country’s population – live in rural America. Rural Americans produce most of our food, much of our energy – and they build strong, cooperative communities. However, they face many challenges when it comes to health and health care. Median income is lower in rural areas, and there’s more poverty. The population is also older and aging rapidly, which means that rural residents will require more health care over time.
Declining health-care infrastructure and low rates of insurance coverage make access to good care even harder. The current situation demands that we study and refine policies that have an impact on rural health.
Q: Is that part of your work at the Sheps Center’s Rural Health Research Center?
 A: At the N.C. Rural Health Research Center, we work to meet those challenges by documenting rural mortality rates across the country, tracking rural hospitals at risk for closure and studying the effects of public insurance coverage on rural Americans.
A: At the N.C. Rural Health Research Center, we work to meet those challenges by documenting rural mortality rates across the country, tracking rural hospitals at risk for closure and studying the effects of public insurance coverage on rural Americans.
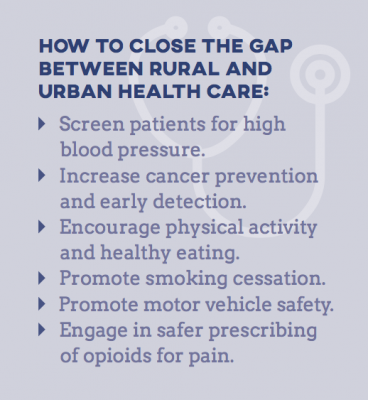
The mortality rate in rural areas is higher than in urban areas – and the gap is growing fast. From 2005 to 2009, rural non-metropolitan areas had a 13 percent higher mortality rate than did urban areas, compared to a 2 percent gap during the period 1990-1992.
Since we know that the root causes of this disparity are different across the country, we’ve tried to document the disparity more clearly, highlighting county-level differences in mortality trends. These more granular data allow us to evaluate the underlying causes of the disparity and provide local policy makers with information they need to devise solutions tailored to their county and region.
Graduate and undergraduate students from the Gillings School have been integral to our work in answering these and other questions.
Q: How concerned are you about the need to increase health-care access and improve insurance coverage for rural Americans?
A: Very. Through our grant funding at the Sheps Center, we’re evaluating access to inpatient care in rural areas through tracking rural hospital closures, monitoring those at-risk for closing and studying innovative solutions to improve access to needed services.
Rural hospital closures are a significant concern across the nation. Since 2010, 81 of more than 2,200 rural hospitals have closed, most of them in the South. To identify areas where hospitals are likely to disappear in the future, Sheps researchers developed a model to determine which hospitals are at risk for closure within two years. The tool provides stakeholders in rural areas with information they need to rally around hospitals in danger of closing.
We’re also actively seeking solutions for areas with a dearth of hospitals and other providers. When a hospital closes, the major concern is that residents won’t have access to emergency services. MedPAC, the entity that advises the Congress on Medicare issues, recently proposed rural freestanding emergency centers – emergency rooms not attached to a hospital – as a potential solution. We don’t know how and whether they’d work in underserved rural communities.
Understanding more about how people access these services will determine whether this is a viable way to expand access to care.
Q: How do we improve insurance coverage?
 A: Ensuring access to services is important, but it is not the full story. People also need access to health insurance to afford needed care. We know that rural communities depend for coverage on public programs, such as Medicare and Medicaid, to a greater degree than do their urban counterparts. With fewer large employers, residents are less likely to obtain health insurance through their jobs.
A: Ensuring access to services is important, but it is not the full story. People also need access to health insurance to afford needed care. We know that rural communities depend for coverage on public programs, such as Medicare and Medicaid, to a greater degree than do their urban counterparts. With fewer large employers, residents are less likely to obtain health insurance through their jobs.
Medicaid covers nearly half of all children in rural areas, compared to less than 40 percent in urban areas. Due to the high Medicaid coverage rate, expansion of the program made available under the Affordable Care Act disproportionately provides substantial assistance in states that implement it. We need more research on promising ways to improve health insurance rates in rural areas.
Rural health comprises a significant amount of our country’s health-care infrastructure. The population in rural areas has higher needs and fewer resources – both in terms of doctors/hospitals and access to health insurance. However, rural communities are resilient, and we – and others – are working to learn more about how policy might pave the way for better health in rural America.
Carolina Public Health is a publication of the University of North Carolina at Chapel Hill Gillings School of Global Public Health. To view previous issues, please visit sph.unc.edu/cph.
